| Vaccination | |
|---|---|
 Child receiving an oral polio vaccine | |
| ICD-9-CM | 99.3-99.5 |
Vaccination is the administration of antigenic material (a vaccine) to stimulate an individual's immune system to develop adaptive immunity to a pathogen. Vaccines can prevent or ameliorate the morbidity from infection. Vaccine efficacy has been widely studied and verified; for example, the influenza vaccine,[1] the HPV vaccine,[2] and the chicken pox vaccine[3]. Vaccination is the most effective method of preventing infectious diseases;[4] widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the restriction of diseases such as polio, measles, tetanus from large areas of the world.
The active agent of a vaccine may be intact but inactivated (non-infective) or attenuated (with reduced infectivity) forms of the causative pathogens, or purified components of the pathogen that have been found to be highly immunogenic (e.g., the outer coat proteins of a virus). Toxoids are produced for the immunization against toxin-based diseases, such as the modification of tetanospasmin toxin of tetanus to remove its toxic effect but retain its immunogenic effect.[5]
Smallpox was likely the first disease people tried to prevent by purposely inoculating themselves with other types of infections,[6][7] and was the first disease for which a vaccine was produced. The smallpox vaccine was designed in 1796 by the British physician Edward Jenner, although at least six people had used the same principles several years earlier.[8] Louis Pasteur furthered the concept through his pioneering work in microbiology. The immunization was called vaccination because it was derived from a virus affecting cows (Latin: vacca—cow).[6][8] Smallpox was a contagious and deadly disease, causing the deaths of 20–60% of infected adults and over 80% of infected children.[9] When it was eventually eradicated in 1979, it had killed an estimated 300–500 million people during the 20th century alone.[10][11][12]
In common speech, 'vaccination' and 'immunization' have a similar meaning. This distinguishes it from inoculation, which uses unweakened live pathogens, although in common usage either is used to refer to an immunization. Vaccination efforts have been met with some controversy since their inception, on scientific, ethical, political, medical safety, religious, and other grounds. In rare cases, vaccinations can injure people and, in the United States, they may receive compensation for those injuries under the National Vaccine Injury Compensation Program. Early success and compulsion brought widespread acceptance, and mass vaccination campaigns were undertaken, which greatly reduced the incidence of many diseases in numerous geographic regions.
Mechanism of function
In the generic sense, the process of artificial induction of immunity, in an effort to protect against infectious disease, works by 'priming' the immune system with an 'immunogen'. Stimulating immune response, via use of an infectious agent, is known as immunization. Vaccinations involve the administration of one or more immunogens, which can be administered in several forms.

Some vaccines are administered after the patient already has contracted a disease. Vaccinia given after exposure to smallpox, within the first three days, is reported to attenuate the disease considerably, and vaccination up to a week after exposure likely offers some protection from disease or may modify the severity of disease.[13] The first rabies immunization was given by Louis Pasteur to a child after he was bitten by a rabid dog. Subsequent to this, it has been found that, in people with uncompromised immune systems, four doses of rabies vaccine over 14 days, wound care, and treatment of the bite with rabies immune globulin, commenced as soon as possible after exposure, is effective in preventing the development of rabies in humans.[14] Other examples include experimental AIDS, cancer and Alzheimer's disease vaccines. The essential empiricism behind such immunizations is that the vaccine triggers an immune response more rapidly than the natural infection itself.
Most vaccines are given by hypodermic injection as they are not absorbed reliably through the intestines. Live attenuated polio, some typhoid and some cholera vaccines are given orally to produce immunity based in the bowel.
Adjuvants and preservatives
Vaccines typically contain one or more adjuvants, used to boost the immune response. Tetanus toxoid, for instance, is usually adsorbed onto alum. This presents the antigen in such a way as to produce a greater action than the simple aqueous tetanus toxoid. People who get an excessive reaction to adsorbed tetanus toxoid may be given the simple vaccine when time for a booster occurs.
In the preparation for the 1990 Gulf campaign, Pertussis vaccine (not acellular) was used as an adjuvant for Anthrax vaccine. This produces a more rapid immune response than giving only the Anthrax, which is of some benefit if exposure might be imminent.
They may also contain preservatives, which are used to prevent contamination with bacteria or fungi. Until recent years, the preservative thiomersal was used in many vaccines that did not contain live virus. As of 2005, the only childhood vaccine in the U.S. that contains thiomersal in greater than trace amounts is the influenza vaccine,[1] which is currently recommended only for children with certain risk factors.[15] Single-dose Influenza vaccines supplied in the UK do not list Thiomersal (its UK name) in the ingredients. Preservatives may be used at various stages of production of vaccines, and the most sophisticated methods of measurement might detect traces of them in the finished product, as they may in the environment and population as a whole.[2]
Vaccination versus inoculation
Many times these words are used interchangeably, as if they were synonyms. In fact, they are different things. As doctor Byron Plant explains: "Vaccination is the more commonly used term, which actually consists of a "safe" injection of a sample taken from a cow suffering from cowpox... Inoculation, a practice probably as old as the disease itself, is the injection of the variola virus taken from a pustule or scab of a smallpox sufferer into the superficial layers of the skin, commonly on the upper arm of the subject. Often inoculation was done "arm to arm" or less effectively "scab to arm"...[16]
Vaccination began in the 18th century with the work of Edward Jenner.[17][18][19]
Types
All vaccinations work by presenting a foreign antigen to the immune system to evoke an immune response, but there are several ways to do this. The four main types that are currently in clinical use are as follows:
- An inactivated vaccine consists of virus or bacteria that are grown in culture and then killed using a method such as heat or formaldehyde. Although the virus or bacteria particles are destroyed and cannot replicate, the virus capsid proteins or bacterial wall are intact enough to be recognized and remembered by the immune system and evoke a response. When manufactured correctly, the vaccine is not infectious, but improper inactivation can result in intact and infectious particles. Since the properly produced vaccine does not reproduce, booster shots are required periodically to reinforce the immune response.
- In an attenuated vaccine, live virus or bacteria with very low virulence are administered. They will replicate, but locally or very slowly. Since they do reproduce and continue to present antigen to the immune system beyond the initial vaccination, boosters may be required less often. These vaccines may be produced by passaging, for example, adapting a virus into different host cell cultures, such as in animals, or at suboptimal temperatures, allowing selection of less virulent strains, or by mutagenesis or targeted deletions in genes required for virulence. There is a small risk of reversion to virulence, which is smaller in vaccines with deletions. Attenuated vaccines also cannot be used by immunocompromised individuals. Reversions of virulence were described for a few attenuated viruses of chickens (infectious bursal disease virus, avian infectious bronchitis virus, avian infectious laryngotracheitis virus [3], avian metapneumovirus [4])[20]
- Virus-like particle vaccines consist of viral protein(s) derived from the structural proteins of a virus. These proteins can self-assemble into particles that resemble the virus from which they were derived but lack viral nucleic acid, meaning that they are not infectious. Because of their highly repetitive, multivalent structure, virus-like particles are typically more immunogenic than subunit vaccines (described below). The human papillomavirus and Hepatitis B virus vaccines are two virus-like particle-based vaccines currently in clinical use.
- A subunit vaccine presents an antigen to the immune system without introducing viral particles, whole or otherwise. One method of production involves isolation of a specific protein from a virus or bacterium (such as a bacterial toxin) and administering this by itself. A weakness of this technique is that isolated proteins may have a different three-dimensional structure than the protein in its normal context, and will induce antibodies that may not recognize the infectious organism. In addition, subunit vaccines often elicit weaker antibody responses than the other classes of vaccines.
A number of other vaccine strategies are under experimental investigation. These include DNA vaccination and recombinant viral vectors.
History
In written history

It is believed likely that some form of inoculation was developed in India or China before the 16th century.[6] Scholar Ole Lund comments: "The earliest documented examples of vaccination are from India and China in the 17th century, where vaccination with powdered scabs from people infected with smallpox was used to protect against the disease. Smallpox used to be a common disease throughout the world and 20% to 30% of infected persons died from the disease. Smallpox was responsible for 8% to 20% of all deaths in several European countries in the 18th century. The tradition of inoculation may have originated in India in 1000 BCE."[21] The mention of inoculation in the Sact'eya Grantham, an Ayurvedic text, was noted by the French scholar Henri Marie Husson in the journal Dictionaire des sciences me`dicales.[22] Almroth Wright, the professor of pathology at Netley, further helped shape the future of vaccination by conducting limited experiments on the professional staff at Netly, including himself. The outcome of these experiments resulted in further development of vaccination in Europe.[23] The Anatolian Ottoman Turks knew about methods of inoculation. This kind of inoculation and other forms of variolation were introduced into England by Lady Montagu, a famous English letter-writer and wife of the English ambassador at Istanbul between 1716 and 1718, who almost died from smallpox as a young adult and was physically scarred from it. She came across the Turkish methods of inoculation, consenting to have her son inoculated by the Embassy surgeon Charles Maitland in the Turkish way. Lady Montagu wrote to her sister and friends in England describing the process in details. On her return to England she continued to propagate the Turkish tradition of inoculation and had many of her relatives inoculated. The breakthrough came when a scientific description of the inoculation operation was submitted to the Royal Society in 1724 by Dr Emmanual Timoni, who had been the Montagu's family physician in Istanbul. Inoculation was adopted both in England and in France nearly half a century before Jenner's famous smallpox vaccine of 1796.[24]
Since then vaccination campaigns have spread throughout the globe, sometimes prescribed by law or regulations (See Vaccination Acts). Vaccines are now used against a wide variety of diseases besides smallpox. Louis Pasteur further developed the technique during the 19th century, extending its use to killed agents protecting against anthrax and rabies. The method Pasteur used entailed treating the agents for those diseases so they lost the ability to infect, whereas inoculation was the hopeful selection of a less virulent form of the disease, and Jenner's vaccination entailed the substitution of a different and less dangerous disease for the one protected against. Pasteur adopted the name vaccine as a generic term in honor of Jenner's discovery.

Prior to vaccination with cowpox, the only known protection against smallpox was inoculation or variolation (Variola - the Smallpox viruses) where a small amount of live smallpox virus was administered to the patient; this carried the serious risk that the patient would be killed or seriously ill. The death rate from variolation was reported to be around a tenth of that from natural infection with Variola, and the immunity provided was considered quite reliable. Factors contributing to the efficacy of variolation probably include the choices of Variola Minor strains used, the relatively low number of cells infected in the first phase of multiplication following initial exposure, and the exposure route used, via the skin or nasal lining rather than inhalation of droplets into the lungs.
Consistency would suggest the activity should have predated Jenner's description of an effective vaccination system, and there is some history relating to opposition to the older and more hazardous procedure of variolation.[25] In modern times, the first vaccine-preventable disease targeted for eradication was smallpox. The World Health Organization (WHO) coordinated the global effort to eradicate this disease. The last naturally occurring case of smallpox occurred in Somalia in 1977.
Maurice Hilleman was the most prolific of inventors of vaccines. He developed successful vaccines for measles, mumps, hepatitis A, hepatitis B, chickenpox, meningitis, pneumonia and Haemophilus influenzae bacteria.[26]
In 1988, the governing body of WHO targeted polio for eradication by 2000. Although the target was missed, eradication is very close. The next eradication target would most likely be measles, which has declined since the introduction of measles vaccination in 1963.
In 2000, the Global Alliance for Vaccines and Immunization was established to strengthen routine vaccinations and introduce new and under-used vaccines in countries with a per capita GDP of under US$1000. GAVI is now entering its second phase of funding, which extends through 2014.
Society and culture
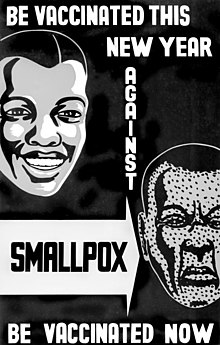
In an attempt to eliminate the risk of outbreaks of some diseases, at various times several governments and other institutions have instituted policies requiring vaccination for all people. For example, an 1853 law required universal vaccination against smallpox in England and Wales, with fines levied on people who did not comply. Common contemporary U.S. vaccination policies require that children receive common vaccinations before entering public school.
Beginning with early vaccination in the nineteenth century, these policies were resisted by a variety of groups, collectively called anti-vaccinationists, who object on scientific, ethical, political, medical safety, religious, and other grounds. Common objections are that vaccinations do not work, that compulsory vaccination represents excessive government intervention in personal matters, or that the proposed vaccinations are not sufficiently safe.[27] Many modern vaccination policies allow exemptions for people who have compromised immune systems, allergies to the components used in vaccinations or strongly held objections.[28]
In countries with limited financial resources, limited coverage is a major problem causing unnecessary morbidity and mortality.[29] More affluent countries are able to subsidize vaccinations for at-risk groups, resulting in more comprehensive and effective cover. In Australia, for example, the Government subsidizes vaccinations for seniors and indigenous Australians.[30]
Public Health Law Research,[31] an independent organization, reported in 2009 that there is insufficient evidence to assess the effectiveness of requiring vaccinations as a condition for specified jobs as a means of reducing incidence of specific diseases among particularly vulnerable populations;[32] that there is sufficient evidence supporting the effectiveness of requiring vaccinations as a condition for attending child care facilities and schools.;[33] and that there is strong evidence supporting the effectiveness of standing orders, which allow healthcare workers without prescription authority to administer vaccine as a public health intervention aimed at increasing vaccination rates.[34]
Allegations of vaccine injuries in recent decades have appeared in litigation in the U.S. Some families have won substantial awards from sympathetic juries, even though most public health officials have said that the claims of injuries were unfounded.[35] In response, several vaccine makers stopped production, which the US government believed could be a threat to public health, so laws were passed to shield makers from liabilities stemming from vaccine injury claims.[35]
Vaccination-autism controversy
One of the most noteworthy allegations of vaccine-induced injury is the MMR vaccine controversy. A 1998 paper by Andrew Wakefield, originally published in The Lancet, presented supposed evidence that the MMR Vaccine (an immunization against measles, mumps and rubella that is typically first administered to children before their first birthday) was linked to the onset of autism spectrum disorders.[36] The article was partially retracted in 2004 by Wakefield's co-authors,[37] and was fully retracted by The Lancet in 2010.[38]
Routes of administration

A vaccine administration may be oral, by injection (intramuscular, intradermal, subcutaneous), by puncture, transdermal or intranasal.[39]
See also
- List of vaccine topics
- H5N1 flu vaccine clinical trials
- Influenza vaccine
- Immunization
- Immunization during pregnancy
- Vaccination and religion
- Vaccination of cats
- Vaccination of dogs
- Vaccine trial
References
- ^ Fiore AE, Bridges CB, Cox NJ (2009). "Seasonal influenza vaccines". Curr. Top. Microbiol. Immunol. Current Topics in Microbiology and Immunology. 333: 43–82. doi:10.1007/978-3-540-92165-3_3. ISBN 978-3-540-92164-6. PMID 19768400.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Chang Y, Brewer NT, Rinas AC, Schmitt K, Smith JS (2009). "Evaluating the impact of human papillomavirus vaccines". Vaccine. 27 (32): 4355–62. doi:10.1016/j.vaccine.2009.03.008. PMID 19515467.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Liesegang TJ (2009). "Varicella zoster virus vaccines: effective, but concerns linger". Can. J. Ophthalmol. 44 (4): 379–84. doi:10.3129/i09-126. PMID 19606157.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ *United States Centers for Disease Control and Prevention (2011). A CDC framework for preventing infectious diseases. Accessed 11 September 2012. “Vaccines are our most effective and cost-saving tools for disease prevention, preventing untold suffering and saving tens of thousands of lives and billions of dollars in healthcare costs each year.”
- American Medical Association (2000). Vaccines and infectious diseases: putting risk into perspective. Accessed 11 September 2012. “Vaccines are the most effective public health tool ever created.”
- Public Health Agency of Canada. Vaccine-preventable diseases. Accessed 11 September 2012. “Vaccines still provide the most effective, longest-lasting method of preventing infectious diseases in all age groups.”
- United States National Institute of Allergy and Infectious Diseases (NIAID). NIAID Biodefense Research Agenda for Category B and C Priority Pathogens. Accessed 11 September 2012. “Vaccines are the most effective method of protecting the public against infectious diseases.”
- ^ http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/tetanus.pdf
- ^ a b c Lombard M, Pastoret PP, Moulin AM (2007). "A brief history of vaccines and vaccination". Rev. - Off. Int. Epizoot. 26 (1): 29–48. PMID 17633292.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Behbehani AM (1983). "The smallpox story: life and death of an old disease". Microbiol. Rev. 47 (4): 455–509. PMC 281588. PMID 6319980.
- ^ a b Plett PC (2006). "[Peter Plett and other discoverers of cowpox vaccination before Edward Jenner]". Sudhoffs Arch (in German). 90 (2): 219–32. PMID 17338405. Retrieved 12 March 2008.
- ^ Riedel S (2005). "Edward Jenner and the history of smallpox and vaccination". Proc (Bayl Univ Med Cent). 18 (1): 21–5. PMC 1200696. PMID 16200144.
- ^ Koplow, David A. (2003). Smallpox: the fight to eradicate a global scourge. Berkeley: University of California Press. ISBN 0-520-24220-3.
- ^ "UC Davis Magazine, Summer 2006: Epidemics on the Horizon". Retrieved 3 January 2008.
- ^ How Poxviruses Such As Smallpox Evade The Immune System, ScienceDaily, February 1, 2008
- ^ "Vaccine Overview" (PDF). Smallpox Fact Sheet. Retrieved 2 January 2008.
- ^ Rupprecht CE, Briggs D, Brown CM; et al. (2010). "Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the advisory committee on immunization practices". MMWR Recomm Rep. 59 (RR–2): 1–9. PMID 20300058.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Melinda Wharton. National Vaccine Advisory committee U.S.A. national vaccine plan
- ^ "Doctors and diagnosis" The difference between Vaccination and Inoculation
- ^ "Edward Jenner - (1749–1823)". Sundaytimes.lk. 2008-06-01. http://sundaytimes.lk/080601/FunDay/famous.html. Retrieved 2009-07-28.
- ^ "History - Edward Jenner (1749 - 1823)". BBC. 2006-11-01. http://www.bbc.co.uk/history/historic_figures/jenner_edward.shtml. Retrieved 2009-07-28.
- ^ "Edward Jenner - Smallpox and the Discovery of Vaccination". http://www.dinweb.org/dinweb/DINMuseum/Edward%20Jenner.asp. Retrieved 2009-07-28.
- ^ Diseases of Poultry, 11th ed. Y. M. Saif et al., editors. Iowa State University Press, Ames, IA, 2003.
- ^ Lund, Ole; Nielsen, Morten Strunge and Lundegaard, Claus (2005). Immunological Bioinformatics. MIT Press. ISBN 0-262-12280-4
- ^ Chaumeton, F.P.; F.V. Me`rat de Vaumartoise. Dictionaire des sciences me`dicales. Paris: C.L.F. Panckoucke, 1812-1822, lvi (1821).
- ^ Curtin, Phillip (1998). "Disease and Empire: The Health of European Troops in the Conquest of Africa". Cambridge University Press. ISBN 0-521-59835-4
- ^ Anthony Henricy (ed.) (1796). Lady Mary Wortley Montagu, Letters of the Right Honourable Lady Mary Wortley Montagu:Written During her Travels in Europe, Asia and Africa. Vol. 1. pp. 167–169.
{{cite book}}:|author=has generic name (help) - ^ Wolfe, Robert M (24 August 2002). "Anti-vaccinationists past and present" (PDF). British Medical Journal. 325 (7361). London: 325. doi:10.1136/bmj.325.7361.430. PMC 1123944. PMID 12193361.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Offit PA (2007). Vaccinated: One Man's Quest to Defeat the World's Deadliest Diseases. Washington, DC: Smithsonian. ISBN 0-06-122796-X.
- ^ Wolfe R, Sharp L (2002). "Anti-vaccinationists past and present". BMJ. 325 (7361): 430–2. doi:10.1136/bmj.325.7361.430. PMC 1123944. PMID 12193361.
- ^ Salmon DA, Teret SP, MacIntyre CR, Salisbury D, Burgess MA, Halsey NA (2006). "Compulsory vaccination and conscientious or philosophical exemptions: past, present, and future". Lancet. 367 (9508): 436–42. doi:10.1016/S0140-6736(06)68144-0. PMID 16458770.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ The fallacy of coverage: uncovering disparities to improve immunization rates through evidence. Results from the Canadian International Immunization Initiative Phase 2 - Operational Research Grants. Sharmila L Mhatre and Anne-Marie Schryer-Roy. BMC International Health and Human Rights 2009, 9(Suppl 1):S1. doi:10.1186/1472-698X-9-S1-S1
- ^ "Time to think about vaccinations again", Medicines Talk, Sydney, 3 February 2010.
- ^ Public Health Law Research
- ^ Laws and Policies Requiring Specified Vaccinations among High Risk Populations
- ^ Vaccination Requirements for Child Care, School and College Attendance
- ^ Standing Orders for Vaccination
- ^ a b Sugarman SD (2007). "Cases in vaccine court—legal battles over vaccines and autism". N Engl J Med. 357 (13): 1275–7. doi:10.1056/NEJMp078168. PMID 17898095.
- ^ Wakefield A, Murch S, Anthony A; et al. (1998). "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 351 (9103): 637–41. doi:10.1016/S0140-6736(97)11096-0. PMID 9500320. Retrieved 5 September 2007.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) (Retracted) - ^ Murch SH, Anthony A, Casson DH et al. (2004). "Retraction of an interpretation". Lancet. 363 (9411): 750. doi:10.1016/S0140-6736(04)15715-2. PMID 15016483.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ The Editors Of The Lancet (2010). "Retraction—Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 375 (9713): 445. doi:10.1016/S0140-6736(10)60175-4. PMID 20137807.
{{cite journal}}:|last1=has generic name (help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help); Unknown parameter|month=ignored (help) - ^ Plotkin, Stanley A. (2006). Mass Vaccination: Global Aspects - Progress and Obstacles (Current Topics in Microbiology & Immunology). Springer-Verlag Berlin and Heidelberg GmbH & Co. K. ISBN 978-3-540-29382-8.
External links
- U.S. government Vaccine Research Center: Information regarding preventive vaccine research studies
- The Vaccine Page links to resources in many countries.
- Immunisation Immunisation schedule for children in the UK. Published by the UK Department of Health.
- CDC.gov - 'National Immunization Program: leading the way to healthy lives', US Centers for Disease Control (CDC information on vaccinations)
- CDC.gov - 'Mercury and Vaccines (Thimerosal)', US Centers for Disease Control
- Immunize.org - Immunization Action Coalition' (nonprofit working to increase immunization rates)
- WHO.int - 'Immunizations, vaccines and biologicals: Towards a World free of Vaccine Preventable Diseases', World Health Organization (WHO's global vaccination campaign website)
- Health-EU Portal Vaccinations in the EU
- History of Vaccines Medical education site from the College of Physicians of Philadelphia, the oldest medical professional society in the US