→Diagnosis: pivot-shift directed to "pivot-shift'. Duplication avoided. Readability improved. |
→Prevention: rewritten. USA Today is not source of scientific information. Consensus statement of International Olympic Committee added |
||
| Line 71: | Line 71: | ||
== Prevention == |
== Prevention == |
||
Interest in reducing non-contact ACL injury has been intense. The striking added liability of female gender in some sports has only added to the enquiry. The International Olympic Committee, after a comprehensive review of preventive strategies has stated: |
|||
Research has shown that the incidence of non-contact ACL injury can be reduced anywhere from 20% to 80% by engaging in regular neuromuscular training that is designed to enhance [[proprioception]], balance, proper movement patterns and muscle strength.<ref>{{cite news |first=Dick |last=Patrick |title=Specific exercises may be key to preventing ACL injuries |url=http://www.usatoday.com/sports/2003-06-24-acl-cover_x.htm |work=USA Today |date=2003-06-24 |accessdate= }}</ref> |
|||
- there is a quantifiable reduction in the risk of ACL in athletes, particularly women, who complete well-designed injury prevention programs. |
|||
- proper neuromuscular training can decrease peak landing forces. |
|||
- training will significantly enhance hamstring strength and power, and reduce hamstring to quadriceps and side-to-side strength imbalances. |
|||
-it is important to increase gluteus medius and hip abductor strength and to address proper deceleration techniques. |
|||
- most programs attempt to alter dynamic loading of the tibiofemoral joint through neuromuscular and proprioceptive training. |
|||
- emphasis is placed on proper landing technique—landing softly on the forefoot and rolling back to the rearfoot, engaging knee and hip flexion upon landing; two-feet landing instead of one feet should be used if possible. |
|||
- in cutting maneuvres, excessive dynamic valgus of the knee upon landing and squatting should be avoided, focusing on the “knee over toe position”.<ref>{{cite journal | title=Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement | author=P Renstrom, A Ljungqvist, E Arendt, B Beynnon, T Fukubayashi, W Garrett, T Georgoulis, T E Hewett, R Johnson, T Krosshaug, B Mandelbaum, L Micheli, G Myklebust, E Roos, H Roos, P Schamasch, S Shultz, S Werner, E Wojtys, L Engebretsen | date=2008 June | journal=Br J Sports Med | volume=42(6) | pages=394-412 | pmcid=PMC3920910 | doi=10.1136/bjsm.2008.048934 }}</ref> |
|||
==Treatment== |
==Treatment== |
||
Revision as of 01:49, 25 August 2014
| Anterior cruciate ligament injury | |
|---|---|
| Specialty | Orthopedic surgery |
The anterior cruciate ligament is an important, internal, stabilizer of the knee joint, restraining hyperextension. It is injured when it's biomechanical limits are exceeded (over stretched), often with a hyperextension mechanism. Formerly, this occurred most often in a sports contact injury, when other structures were frequently involved. A particularly severe form of the contact injury is called the "unhappy triad" or "O'Donaghue's triad", and involves the anterior cruciate ligament, the medial collateral ligament, and the lateral meniscus. Now, Acl injury is more commonly a non-contact injury, such as a dismount from a layup in basketball. Both forms occur more frequently in athletes than in the general population and are prevalent in alpine skiing, Association football, American football, Australian rules football, basketball, rugby, professional wrestling, martial arts, and artistic gymnastics.[1] It is also known to be about three times more common in women than men.[1]
The consequences of the injury depend on how much the stability of the knee is affected, and the extent to which other structures have been involved, and this can vary on a case-by-case basis. If instability is evident, particularly rotatory instability, then the menisci will get injured, sooner or later, setting the scene for progressive, degenerative, arthritis of the knee.
Signs and symptoms
The combination of "pop" during a twisting movement, together with inability to continue participation, and followed by early swelling is said to indicate a 90% probability of rupture of the anterior cruciate ligament.[2]
Causes
ACL injuries occur when an individual stops suddenly or plants their foot hard into the ground (cutting). ACL failure has been linked to heavy or stiff-legged landing; the knee rotating while landing, especially when the knee is in an unnatural position.
Women in sports such as association football, basketball, and tennis are significantly more prone to ACL injuries than men. The discrepancy has been attributed to gender differences in anatomy, general muscular strength, reaction time of muscle contraction and coordination, and training techniques. Women have a relatively wider pelvis, requiring the femur to angle toward the knees.[3] The role of genetics is currently speculative.
The majority of ACL injuries occur in athletes landing flat on their heels. The latter directs the forces directly up the tibia into the knee, while the straight-knee position places the anterior femoral condyle on the back-slanted portion of the tibia. The resultant forward slide of the tibia relative to the femur is restrained primarily by the now-vulnerable ACL.
Ligament Dominance
The increased risk of anterior cruciate ligament injury among female athletes is best predicted by the motion and loading of the knee during performance situations.[4] The ligament dominance theory suggests that females typically perform athletic movements with greater knee valgus angles. A greater amount of stress is placed on the ACL in these situations because there is high activation of the quadriceps muscles despite limited knee flexion, limited hip flexion, greater hip adduction, and a large knee adductor moment.[5][6] Additionally, females typically land with their tibia rotated internally or externally.[7] As a result of increased knee valgus stress, ground reaction forces are greater and laterally directed.[8]
Quadriceps Dominance
Ligament dominance is observed when there is excessive movement in the frontal plane to accommodate limited movement in the sagittal plane. This is caused by weakness in the hamstring muscles or reliance on the strength of the quadriceps muscles.[6] This quadriceps dominance theory identifies when the hamstring muscles are notably weaker than the quadriceps muscles. As a result, knee stability in performance situations depends on the quadriceps due to a discrepancy in the pattern in recruiting quadriceps and hamstring muscles.[9]
Trunk and Leg Dominance
Other theories used to explain the increased risk of ACL injury among female athletes include the trunk dominance and leg dominance theories. Trunk dominance suggests that males typically exhibit greater control of the trunk in performance situations as evidenced by greater activation of the internal oblique muscle. Leg dominance suggests that females exhibit greater kinematic leg asymmetry in knee valgus angles, hip abduction, and ankle abduction in performance situations.[5]
-
Right knee-joint, from the front, showing interior ligaments.
-
Left knee-joint from behind, showing interior ligaments.
Evolution
ACL tears occur for two reasons: the failure load of the ligament and the mechanical load applied to it. Female ACLs will fail at relatively lower loads than males, and female pelvic anatomy also predisposes women to higher mechanical loads on the knee. The combination of these factors leads to an increased likelihood – four to six times – for females to tear their ACLs than males.[10]
There are both proximate and ultimate causes for the increased susceptibility of women to ACL tears. Proximate, or immediate, causation is that women have wider pelvises than men. This widened pelvis creates a wider valgus knee angle: with wider hips, the femur must angle towards the knee at a wider angle. This difference in skeletal anatomy between men and women makes women more susceptible to ACL tears due to greater rotational force placed upon the knee.[11]
Underlying this proximate cause is the ultimate cause of male and female anatomical divergence due to the influence of sex hormones. Before puberty, there is no observed difference in frequency of ACL tears between the sexes. Changes in sex hormones, specifically increased estrogen and progesterone in women, make possible many of the anatomical changes necessary for successful reproduction and childbirth. Through the influence of sex hormones, female pelvises widen during puberty. The proximate cause of increased likelihood of ACL tears in women thus stems from the ultimate cause of differences in sex hormones between males and females.
During puberty, sex hormones also affect the remodeled shape of soft tissues throughout the body. The tissue remodeling results in female ACLs that are smaller and will fail (i.e. tear) at lower loading forces. Sex hormones, the ultimate cause of ACL tear differences, create differences in ligament and muscular stiffness between men and women. Women’s knees are less stiff than men’s during muscle activation. Force applied to a less stiff knee is more likely to result in ACL tears.[10]
While these sex hormones may appear detrimental to women in terms of sports injuries, they are necessary for childbirth and thus are an intrinsic part of the evolution of the human species. Females face an evolutionary trade-off in anatomy between a body adapted for efficient bipedal movement and one adapted for successful childbirth. Trade-offs, a common theme in the history of human evolution, occur when humans evolve a change in physiology in order to reduce illness or injury (in this case, death in childbirth). This change may have deleterious effects on another aspect of human physiology: in the case of pelvic anatomy, a too-wide pelvis would not be able to be supported by gluteal muscles and would be an inefficient means of bipedal locomotion.
Applied to female pelvic width, a narrower pelvis would reduce valgus knee angle, leading, among other things, to lower rates of ACL tears and other physical benefits like a more efficient stride and running gait. Yet this narrow pelvis would constrain childbirth, possibly resulting in the death of the mother and child. Thus, throughout human history, women with wider pelvises had higher rates of survival in childbirth and passed on these wider-hipped genes to their offspring.
Pelvic width was constrained by the trade-off between locomotion and childbirth: wider pelvises offered a fitness advantage up to a certain point, where they became a liability due to decreased bipedal abilities. Pelvic width thus could not expand as wide as it might to make childbirth easier, due to the necessity of human bipedal locomotion. Humans evolved from quadruped primates who had only the physiological capabilities for inefficient, infrequent bipedal locomotion. Evolutionary adaptations like larger, more powerful gluteal muscles allowed humans to stabilize their hips and trunk during bipedal locomotion. Multiple theories exist about why bipedalism conferred a reproductive advantage. Bipedalism allowed humans to use their hands to carry food, was a more efficient form of long-distance transportation than quadrupedal locomotion, improved thermoregulation by reducing the amount of skin exposed to direct sunlight (the top of the head vs. the entire back), and permitted humans to engage in persistence hunting. East Africa was changing from a forest to a grassland when bipedalism first evolved in humans' ancestors approximately 8 million years ago, and the new behaviors it enabled them to engage in would have made them better fit to survive in this changed environment.[12]
Thus female pelvic width is a trade-off, where childbirth is easier but not as easy as it might be in other quadruped primates; and bipedal locomotion is efficient but not as efficient as it might be with narrower hips. These sex differences in locomotion underlie differential rates of ACL injury in men and women.
Diagnosis
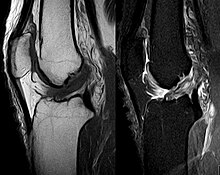
The pivot-shift test, anterior drawer test and Lachman test are used during the clinical examination of suspected ACL injury. The Lachman test is recognized by most authorities as the most reliable and sensitive test, and usually superior to the anterior drawer test.[13] The ACL can also be visualized using a magnetic resonance imaging scan (MRI scan).
An ACL tear can present with a popping sound heard after impact, swelling after a couple of hours, severe pain when bending the knee, and buckling or locking of the knee during movement.
Though clinical examination in experienced hands can be accurate, the diagnosis is usually confirmed by MRI, which has greatly lessened the need for diagnostic arthroscopy and which has a higher accuracy than clinical examination. It may also permit visualization of other structures which may have co-incidentally involved, such as a meniscus, or collateral ligament, or posterolateral corner of the knee joint.
Prevention
Interest in reducing non-contact ACL injury has been intense. The striking added liability of female gender in some sports has only added to the enquiry. The International Olympic Committee, after a comprehensive review of preventive strategies has stated: - there is a quantifiable reduction in the risk of ACL in athletes, particularly women, who complete well-designed injury prevention programs. - proper neuromuscular training can decrease peak landing forces. - training will significantly enhance hamstring strength and power, and reduce hamstring to quadriceps and side-to-side strength imbalances. -it is important to increase gluteus medius and hip abductor strength and to address proper deceleration techniques. - most programs attempt to alter dynamic loading of the tibiofemoral joint through neuromuscular and proprioceptive training. - emphasis is placed on proper landing technique—landing softly on the forefoot and rolling back to the rearfoot, engaging knee and hip flexion upon landing; two-feet landing instead of one feet should be used if possible. - in cutting maneuvres, excessive dynamic valgus of the knee upon landing and squatting should be avoided, focusing on the “knee over toe position”.[14]
Treatment
The ACL primarily serves to stabilize the knee in an extended position and when surrounding muscles are relaxed; so if the muscles are strong, many people can function without it.
The term for non-surgical treatment for ACL rupture is "conservative management", and it often includes physical therapy and using a knee brace. Lack of an ACL increases the risk of other knee injuries such as a torn meniscus, so sports with cutting and twisting motions are strongly discouraged. For patients who frequently participate in such sports, surgery is often indicated.
Patients who have suffered an ACL injury should always be evaluated for other knee injuries that often occur in combination with an ACL tear. These include cartilage/meniscus injuries, bone bruises, PCL tears, posterolateral injuries and collateral ligament injuries.
Conservative
A torn ACL is less likely to restrict the movement of the knee. When tears to the ACL are not repaired it can sometimes cause damage to the cartilage inside the knee because with the torn ACL the tibia and femur bone are more likely to rub against each other. Immediately after the tear of the ACL, the person should rest the knee, ice it every 15 to 20 minutes, provide compression on the knee, and then elevate above the heart; this process helps decrease the swelling and reduce the pain. The form of treatment is determined based on the severity of the tear on the ligament. Small tears in the ACL may just require several months of rehab in order to strengthen the surrounding muscles, the hamstring and the quadriceps, so that these muscles can compensate for the torn ligament. Falls associated with knee instability may require the use of a specific brace to stabilize the knee. Women are more likely to experience falls associated with the knee giving way. Sudden falls can be associated with further complications such as fractures and head injury.
Surgery
If the tear is severe, surgery may be necessary because the ACL cannot heal independently, as there is no blood supply to this ligament. Surgery is usually required among athletes because the ACL is needed in order to perform sharp movements safely and with stability. The reconstructive surgery is usually done several weeks after the injury in order to allow the swelling and inflammation to go down. During surgery the ACL is not repaired, instead, it is reconstructed using other tendons in the body. There are three different types of ACL surgery. Patella tendon-bone auto graft and hamstring auto graft are the most common and preferred and tend to produce the best results. For the Patella tendon-bone auto graft, the central 1/3 of the patella tendon is removed along with a piece of bone at the attachment sites on the kneecap and tibia. The advantages of using this method is that the patella tendon and ACL are relatively the same length and it uses a bone to bone attachment which most surgeons agree is much stronger than other healing methods. Disadvantages of this method is common anterior knee pain due to the removal of bone from the kneecap. For the hamstring auto graft, two tendons are taken from the hamstring muscles and wrapped together to form the new ACL. Advantages of this method are less pain associated with post surgery healing than that of the patella tendon-bone graft due to the fact no bone is removed, and the small incision. The disadvantage of this method is that the new ligament takes longer to heal since there is no bone to bone healing and the tendon to bone connection takes relatively long to become rigid.[15] After the surgery, rehabilitation is required in order to strengthen the surrounding muscles and stabilize the joint.
There are two main options for ACL graft selection, allograft and autograft. Autografts are the person's own tissues, and options include the hamstring tendons or middle third of the patella tendon but it is not known which is best.[16] Allografts are cadaveric tissue sourced from a tissue bank. Each method has its own advantages and disadvantages; hamstring and middle third of patella tendon having similar outcomes. Patellar grafts are often incorrectly cited as being stronger, but the site of the harvest is often extremely painful for weeks after surgery and some patients develop chronic patellar tendinitis. Replacement via a posthumous donor involves a slightly higher risk of infection. Additionally, donor grafts eliminate tendon harvesting which, due to improved arthroscopic methods, is responsible for most post-operative pain.
The surgery is typically undertaken arthroscopically, with tunnels drilled into the femur and tibia at approximately the original ACL attachments. The graft is then placed into position and held in place. There are a variety of fixation devices available, particularly for hamstring tendon fixation. These include screws, buttons and post fixation devices. The graft typically attaches to the bone within six to eight weeks.[citation needed] The original collagen tissue in the graft acts as a scaffold and new collagen tissue is laid down in the graft with time. Hence the graft takes over six months to reach maximal strength.[citation needed]
After surgery, the knee joint loses flexibility, and the muscles around the knee and in the thigh tend to atrophy. All treatment options require extensive physical therapy to regain muscle strength around the knee and restore range of motion (ROM). For some patients, the lengthy rehabilitation period may be more difficult to deal with than the actual surgery. In general, a rehabilitation period of six months to a year is required to regain pre-surgery strength and use. [citation needed] This is very dependent on the rehabilitation assignment provided by the surgeon as well as the person who is receiving the surgery. External bracing is recommended for athletes in contact and collision sports for a period of time after reconstruction. It is important however to realize that this type of prevention is given by a 'surgeon to surgeon' basis; all surgeons will prescribe a brace and crutches for post surgery recovery. Total usage time is one month. After surgery, no sports are allowed for 6 to 7 months. Whether the ACL deficient knee is reconstructed or not, the patient is susceptible to early onset of chronic degenerative joint disease.
Rehabilitation
The rehabilitation process is a very important to reconstruction. The process to regain full use of the joint is long and rigorous. The doctor will start the patient on the rehabilitation program, which is broken down into phases:
Phase 1: Early rehabilitation consists of short-term management, i.e. management of pain and swelling while regaining movement.
Phase 2: In weeks 3 and 4, the pain should be subsiding and the patient will be ready to try more things on an unsteady knee. Joint protection during this step is emphasized. The patient will be able to start doing exercises such as mini wall sits and riding stationary bikes. The aim is to be able to bend the knee 100 degrees.
Phase 3: Weeks 4 and 6 are the controlled ambulation phase. At this point the patient will be doing the exercises from phase 2 plus some more challenging ones. The patient will try to get their knee to bend 130 degrees during this stage. The aim during this period is to focus heavily on improving balance.
Phase 4: This is the moderate protection phase, covering weeks 6 to 8. In this period the patient will try to obtain full range of motion as well as increase resistance for the workouts.
Phase 5: This is the light activity phase, covering weeks 8 to 10. Rehabilitation during period places particular emphasis on strengthening exercises, with increased concentration on balance and mobility.
Phase 6: This is the return to activity phase, lasting from week 10 until the target activity level is reached. At this point the patient will be able to start jogging and performing moderately intense agility drills. Somewhere between month 3 and month 6 the surgeon will probably request that the patient perform physical tests to monitor the activity level. When the doctor feels comfortable with the progress of the patient, s/he will clear that person to resume a fully active lifestyle.[17]
Epidemiology
Gender difference in ACL tears in relationship with physical activities have been asserted.[18] The researchers performed an epidemiology study on young athletic populations. Previous studies found that women that participate in the same physical activities as men are more at risk for ACL injuries. “The NCAA statistics have shown that, when compared with male athletes who participate in activities with similar rules and equipment, female athletes are two to eight times more likely to sustain an ACL injury”.[19] The authors hypothesize that the frequency rate for males and females in the athletic and college aged population is the same. The study looked at college graduation classes from 1994-2003 at major institutions. The players who received a whole tear were examined for apparatus of injury and the type of sport they played when the injury occurred. The authors calculated the accident rate, opinion of danger, gender incidents, class year, and the accident rate differentiating men and women. There were 353 ACL injuries in 10 classes during the span of the study. The researchers calculated a 4-year accident proportion of 3.24 per 100 students for men, and 3.51 for women. Overall, the ACL injury rate not including male-only sports was substantially greater in women with an incidence ratio of 1.51 (pg 5). Women are more likely to get injured at gymnastics courses with an incidence ratio of 5.67; with an indoor obstacle course test the rate is 3.72; and there is a 2.42 incidence ratio on basketball. The authors concluded that there is slim gender difference in gender ACL tear. On the other hand, there were significant gender differences in ACL injury rates when particular specific sports and physical activities were compared.
A notable finding is that women are three times more likely to have an ACL injury than men, due to variations of hormone levels and greater ligament strength in men than in women. “The IR (incidence rate) of ACL reconstructions was clearly increasing in the female population. The largest increase was in female high school students…”.[20] Most importantly, there is substantial difference in neuromuscular coordination and control in landing—women have less hip and knee flexion. Women also have wider Q angles than men, and this combined with their weaker hip strength makes them more prone to an ACL tear. “One of the anatomical factors that is the subject of considerable debate is the morphology of the femoral intercondylar notch, and the relationship between notch width and disruption of the ACL”.[21] Gabos states that having a smaller notch width leads to higher chances of injuring and tearing the ACL. The type of sport that an individual participates in could also lead toward ACL tears, “Seventy percent of ACL injuries occur during athletic participation, and they are most common in sports that require rapid stopping, cutting, and changing direction…”.[19] Sports like soccer and basketball fall into this category perfectly. This is seen especially in Women's Basketball and Volleyball. Athletic trainers and team physicians advise female athletes to adapt an ACL conditioning program.
References
- ^ a b Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K (Dec 2007). "A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen". Arthroscopy. 23(12): 1320–25. PMID 18063176.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bytomski J, Moorman C (2010). Oxford American Handbook of Sports Medicine. Oxford American Handbook of Medicine Series (First ed.). Oxford, New York: Oxford University Press. p. 290. ISBN 9780195372199.
- ^ McLean SG, Huang X, van den Bogert AJ (2005). "Association between lower extremity posture at contact and peak when the tibia moves too far forward implications for ACL injury". Clin Biomech (Bristol, Avon). 20 (8): 863–70. doi:10.1016/j.clinbiomech.2005.05.007. PMID 16005555.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hewett, T. E., Myer, G. D., Ford, K. R., Heidt, R. S., Colosimo, A. J., McLean, S. G., van den Bogert, A. J., Paterno, M. V., and Succop, P. (2005). Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. The American Journal of Sports Medicine, 33(4), 492-501.
- ^ a b Pappas, E., and Carpes, F. P. (2012). Lower extremity kinematic asymmetry in male and female athletes performing jump-landing tasks. Journal of Science and Medicine in Sport, 15(1), 87-92.
- ^ a b Pollard, C. D., Sigward, S. M., and Powers, C. M. (2010). Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clinical Biomechanics, 25(2), 142-146.
- ^ Nagano, Y., Ida, H., Akai, M., and Fukubayashi, T. (2007). Gender differences in knee kinematics and muscle activity during single limb drop landing. The Knee, 14(3), 218-223.
- ^ Sigward, S. M., and Powers, C. M. (2007). Loading characteristics of females exhibiting excessive valgus moments during cutting. Clinical Biomechanics, 22(7), 827-833.
- ^ Ford, K. R., Myer, G. D., and Hewett, T. E. (2003). Valgus knee motion during landing in high school female and male basketball players. Medicine and Science in Sports and Exercise, 31(10), 1745-1750.
- ^ a b Slauterbeck, JR; Hickox JR; Beynnon B; Hardy DM (2006). "Anterior Cruciate Ligament Biology andIts Relationship to Injury Forces". Orthop Clin N Am. 37: 585–591.
{{cite journal}}:|access-date=requires|url=(help) - ^ Hewitt, Timothy E.; Ford KR; Hoogenboom BJ; Myer GD (December 2010). "UNDERSTANDING AND PREVENTING ACL INJURIES: CURRENT BIOMECHANICAL AND EPIDEMIOLOGIC CONSIDERATIONS - UPDATE 2010". N Am J Sports Phys Ther. 5 (4): 234–251. PMC 3096145. PMID 21655382.
- ^ Rob DeSalle; Ian Tattersall (2008). Human origins: what bones and genomes tell us about ourselves. Texas A&M University Press. p. 146. ISBN 978-1-58544-567-7. Retrieved 28 October 2013.
- ^ van Eck CF, van den Bekerom MP, Fu FH, Poolman RW, Kerkhoffs GM (Aug 2013). "Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of physical examinations with and without anaesthesia". Knee Surg Sports Traumatol Arthrosc. 21(8): 1895–903. doi:10.1007/s00167-012-2250-9. PMID 23085822.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ P Renstrom, A Ljungqvist, E Arendt, B Beynnon, T Fukubayashi, W Garrett, T Georgoulis, T E Hewett, R Johnson, T Krosshaug, B Mandelbaum, L Micheli, G Myklebust, E Roos, H Roos, P Schamasch, S Shultz, S Werner, E Wojtys, L Engebretsen (2008 June). "Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement". Br J Sports Med. 42(6): 394–412. doi:10.1136/bjsm.2008.048934.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|pmcid=ignored (|pmc=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Cluett, Jonathan (7 September 2010). "ACL Reconstruction". About.com. New York Times Company.
- ^ Mohtadi, NG (Sep 7, 2011). "Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults". Cochrane Database of Systematic Reviews. 9 (9): CD005960. doi:10.1002/14651858.CD005960.pub2. PMID 21901700.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ http://www.ehealthmd.com/library/acltears/ACL_rehab.html
- ^ Mountcastle SB, Posner M, Kragh JF, Taylor DC (October 2007). "Gender differences in anterior cruciate ligament injury vary with activity: epidemiology of anterior cruciate ligament injuries in a young, athletic population". Am J Sports Med. 35 (10): 1635–42. doi:10.1177/0363546507302917. PMID 17519438.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b (Guigliano and Solomon, 2007)
- ^ (Csintalan et al, 2008)
- ^ (Gabos et al, 2010)
External links
- Educational site
- The Knee Library — Articles pertaining to knee injuries
- Knee Treatment Blog
- Vermont Safety Research — Tips for knee friendly skiing
- ACL Injury in Martial Arts
- Torn ACL prevention and recovery
- ACL Injury Prevention – The Evidence Mounts, Science of Soccer Online
- ACL Injury — A simple patient guide.

