 | |
| Clinical data | |
|---|---|
| Trade names | Bromfed, Dimetapp, Bromfenex, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682545 |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Liver |
| Elimination half-life | 24.9 ± 9.3 hours[1] |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.001.507 |
| Chemical and physical data | |
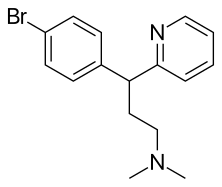
| Formula | C16H19BrN2 |
| Molar mass | 319.246 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Brompheniramine, sold under the brand name Dimetapp among others, is a first-generation antihistamine drug of the propylamine (alkylamine) class.[2] It is indicated for the treatment of the symptoms of the common cold and allergic rhinitis, such as runny nose, itchy eyes, watery eyes, and sneezing. Like the other first-generation drugs of its class, it is considered a sedating antihistamine.[2]
It was patented in 1948 and came into medical use in 1955.[3] In 2021, the combination with dextromethorphan and pseudoephedrine was the 294th most commonly prescribed medication in the United States with more than 500,000 prescriptions.[4][5]
Side effects[edit]
Brompheniramine's effects on the cholinergic system may include side-effects such as drowsiness, sedation, dry mouth, dry throat, blurred vision, and increased heart rate. It is listed as one of the drugs of highest anticholinergic activity in a study of anticholinergenic burden, including long-term cognitive impairment.[6]
Pharmacology[edit]
Brompheniramine works by acting as an antagonist of histamine H1 receptors. It also functions as a moderately effective anticholinergic agent, and is likely an antimuscarinic agent similar to other common antihistamines such as diphenhydramine.
Brompheniramine is metabolised by cytochrome P450 isoenzymes in the liver.
Chemistry[edit]
Brompheniramine is part of a series of antihistamines including pheniramine (Naphcon) and its halogenated derivatives and others including fluorpheniramine, chlorpheniramine, dexchlorpheniramine (Polaramine), triprolidine (Actifed), and iodopheniramine. The halogenated alkylamine antihistamines all exhibit optical isomerism; brompheniramine products contain racemic brompheniramine maleate, whereas dexbrompheniramine (Drixoral) is the dextrorotary (right-handed) stereoisomer.[2][7]
Brompheniramine is an analog of chlorpheniramine. The only difference is that the chlorine atom in the benzene ring is replaced with a bromine atom. It is also synthesized in an analogous manner.[8][9]
History[edit]
Arvid Carlsson and his colleagues, working at the Swedish company Astra AB, were able to derive the first marketed selective serotonin reuptake inhibitor, zimelidine, from brompheniramine.[10]
Names[edit]
Brand names include Bromfed, Dimetapp, Bromfenex, Dimetane, and Lodrane. All bromphemiramine preparations are marketed as the maleate salt.[2]
References[edit]
- ^ Simons FE, Frith EM, Simons KJ (December 1982). "The pharmacokinetics and antihistaminic effects of brompheniramine". The Journal of Allergy and Clinical Immunology. 70 (6): 458–64. doi:10.1016/0091-6749(82)90009-4. PMID 6128358.
- ^ a b c d Sweetman SC, ed. (2005). Martindale: the complete drug reference (34th ed.). London: Pharmaceutical Press. p. 569–70. ISBN 0-85369-550-4. OCLC 56903116.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 546. ISBN 9783527607495.
- ^ "The Top 300 of 2021". ClinCalc. Archived from the original on 15 January 2024. Retrieved 14 January 2024.
- ^ "Brompheniramine; Dextromethorphan; Pseudoephedrine - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ Salahudeen MS, Duffull SB, Nishtala PS (March 2015). "Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review". BMC Geriatrics. 15 (31): 31. doi:10.1186/s12877-015-0029-9. PMC 4377853. PMID 25879993.
- ^ Troy DB, Beringer P (2006). Remington: The Science and Practice of Pharmacy. Lippincott Williams & Wilkins. pp. 1546–8. ISBN 9780781746731.
- ^ US 3061517, Walter LA, issued 1962.
- ^ US 3030371, Walter LA, issued 1962.
- ^ Barondes SH (2003). Better Than Prozac. New York: Oxford University Press. pp. 39–40. ISBN 0-19-515130-5.