 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Clarinex, Aerius, Allex, others[1][2] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a602002 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth (tablets, solution) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Rapidly absorbed |
| Protein binding | 83 to 87% |
| Metabolism | UGT2B10, CYP2C8 |
| Metabolites | 3-Hydroxydesloratadine |
| Onset of action | within 1 hour[3] |
| Elimination half-life | 27 hours[3] |
| Duration of action | up to 24 hours[3] |
| Excretion | 40% as conjugated metabolites into urine Similar amount into the feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.166.554 |
| Chemical and physical data | |
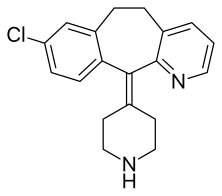
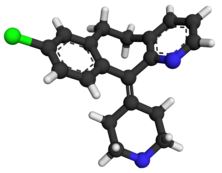
| Formula | C19H19ClN2 |
| Molar mass | 310.83 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Desloratadine (trade names Clarinex and Aerius) is a tricyclic H1 inverse agonist that is used to treat allergies. It is an active metabolite of loratadine.[3]
It was patented in 1984 and came into medical use in 2001.[4]
Medical uses[edit]
Desloratadine is used to treat allergic rhinitis, nasal congestion and chronic idiopathic urticaria (hives).[5] It is the major metabolite of loratadine and the two drugs are similar in safety and effectiveness.[5] Desloratadine is available in many dosage forms and under many trade names worldwide.[6]
An emerging indication for desloratadine is in the treatment of acne, as an inexpensive adjuvant to isotretinoin and possibly as maintenance therapy or monotherapy.[7][8]
Side effects[edit]
The most common side-effects are fatigue (1.2%[9]), dry mouth (3%[9]), and headache (0.6%[9]).[5]
Interactions[edit]
Co-administration with erythromycin, ketoconazole, azithromycin, fluoxetine or cimetidine resulted in elevated blood plasma concentrations of desloratadine and its metabolite 3-hydroxydesloratadine in studies. However, no clinically relevant changes were observed.[10][11]
Pharmacology[edit]
Pharmacodynamics[edit]
Desloratadine is a selective H1-antihistamine which functions as an inverse agonist at the histamine H1 receptor.[12]
At very high doses, is also an antagonist at various subtypes of the muscarinic acetylcholine receptors. This effect is not relevant for the drug's action at therapeutic doses.[13]
Pharmacokinetics[edit]
Desloratadine is well absorbed from the gut and reaches highest blood plasma concentrations after about three hours. In the bloodstream, 83 to 87% of the substance are bound to plasma proteins.[11]
Desloratadine is metabolized to 3-hydroxydesloratadine in a three-step sequence in normal metabolizers. First, n-glucuronidation of desloratadine by UGT2B10; then, 3-hydroxylation of desloratadine N-glucuronide by CYP2C8; and finally, a non-enzymatic deconjugation of 3-hydroxydesloratadine N-glucuronide.[14] Both desloratadine and 3-hydroxydesloratadine are eliminated via urine and feces with a half-life of 27 hours in normal metabolizers.[11][15]

It exhibits only peripheral activity since it does not readily cross the blood–brain barrier; hence, it does not normally cause drowsiness because it does not readily enter the central nervous system.[16]
Desloratadine does not have a strong effect on a number of tested enzymes in the cytochrome P450 system. It was found to weakly inhibit CYP2B6, CYP2D6, and CYP3A4/CYP3A5, and not to inhibit CYP1A2, CYP2C8, CYP2C9, or CYP2C19. Desloratadine was found to be a potent and relatively selective inhibitor of UGT2B10, a weak to moderate inhibitor of UGT2B17, UGT1A10, and UGT2B4, and not to inhibit UGT1A1, UGT1A3, UGT1A4, UGT1A6, UGT1A9, UGT2B7, UGT2B15, UGT1A7, and UGT1A8.[14]
Pharmacogenomics[edit]
2% of Caucasian people and 18% of people from African descent are desloratadine poor metabolizers. In these people, the drug reaches threefold highest plasma concentrations six to seven hours after intake, and has a half-life of about 89 hours. However, the safety profile for these subjects is not worse than for extensive (normal) metabolizers.[11][15]
See also[edit]
References[edit]
- ^ Murdoch D, Goa KL, Keam SJ (April 7, 2003). "Desloratadine: an update of its efficacy in the management of allergic disorders". Drugs. 63 (19): 2051–2077. doi:10.2165/00003495-200363190-00010. PMID 12962522. S2CID 195689362.
- ^ "Allex EPAR". European Medicines Agency (EMA).
- ^ a b c d Lieberman P, Hernandez-Trujillo V, Lieberman J, Frew AJ (2008). "Antihistamines". Clinical Immunology. Elsevier. pp. 1317–1329. doi:10.1016/b978-0-323-04404-2.10089-2. ISBN 9780323044042.
Desloratadine is a metabolite of loratadine. The onset of action is within 1 hour. Peak serum concentrations of desloratadine appear 3 hours after dosing. The mean elimination half-life of desloratadine is 27 hours and that of its metabolite is 36 hours. The consumption of food does not interfere with the absorption of desloratadine. Wheal inhibition is detected 1 hour after administration and may last 24 hours.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 549. ISBN 9783527607495.
- ^ a b c See S (November 2003). "Desloratadine for allergic rhinitis". American Family Physician. 68 (10): 2015–2016. PMID 14655812. Archived from the original on 2005-07-24. Retrieved 2005-08-01.
- ^ Drugs.com Desloratadine entry at drugs.com international Page accessed May 4, 2015
- ^ Lee HE, Chang IK, Lee Y, Kim CD, Seo YJ, Lee JH, Im M (December 2014). "Effect of antihistamine as an adjuvant treatment of isotretinoin in acne: a randomized, controlled comparative study". Journal of the European Academy of Dermatology and Venereology. 28 (12): 1654–1660. doi:10.1111/jdv.12403. PMID 25081735. S2CID 3406128.
- ^ Layton AM (April 2016). "Top Ten List of Clinical Pearls in the Treatment of Acne Vulgaris". Dermatologic Clinics. 34 (2): 147–157. doi:10.1016/j.det.2015.11.008. PMID 27015774.
- ^ a b c González-Núñez V, Valero A, Mullol J (May 2013). "Safety evaluation of desloratadine in allergic rhinitis". Expert Opinion on Drug Safety. 12 (3). Informa Healthcare: 445–453. doi:10.1517/14740338.2013.788148. PMID 23574541. S2CID 40472187.
- ^ "Clarinex: Prescribing Information" (PDF). U.S. Food and Drug Administration. Retrieved 2022-01-21.
- ^ a b c d "Aerius: EPAR – Product Information" (PDF). European Medicines Agency. Archived from the original (PDF) on 2019-07-05. Retrieved 2022-01-21.
- ^ Canonica GW, Blaiss M (February 2011). "Antihistaminic, anti-inflammatory, and antiallergic properties of the nonsedating second-generation antihistamine desloratadine: a review of the evidence". The World Allergy Organization Journal. 4 (2): 47–53. doi:10.1097/WOX.0b013e3182093e19. PMC 3500039. PMID 23268457.
- ^ "Aerius: EPAR – Scientific Discussion" (PDF). European Medicines Agency. 2006-04-03. Archived from the original (PDF) on 2018-03-16. Retrieved 2017-10-13.
- ^ a b Kazmi F, Yerino P, Barbara JE, Parkinson A (September 2015). "Further Characterization of the Metabolism of Desloratadine and Its Cytochrome P450 and UDP-glucuronosyltransferase Inhibition Potential: Identification of Desloratadine as a Relatively Selective UGT2B10 Inhibitor". Drug Metabolism and Disposition. 43 (9): 1294–1302. doi:10.1124/dmd.115.065011. PMID 26135009.
- ^ a b Drugs.com: Desloratadine Monograph.
- ^ Mann RD, Pearce GL, Dunn N, Shakir S (April 2000). "Sedation with "non-sedating" antihistamines: four prescription-event monitoring studies in general practice". BMJ. 320 (7243): 1184–1186. doi:10.1136/bmj.320.7243.1184. PMC 27362. PMID 10784544.
External links[edit]
- "Desloratadine". Drug Information Portal. U.S. National Library of Medicine.