| FGF21 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | FGF21, fibroblast growth factor 21 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 609436 MGI: 1861377 HomoloGene: 10428 GeneCards: FGF21 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Fibroblast growth factor 21 is a protein that in mammals is encoded by the FGF21 gene.[5][6] The protein encoded by this gene is a member of the fibroblast growth factor (FGF) family and specifically a member of the endocrine subfamily which includes FGF23 and FGF15/19. FGF21 is the primary endogenous agonist of the FGF21 receptor, which is composed of the co-receptors FGF receptor 1 and β-Klotho.[7]
FGF family members possess broad mitogenic and cell survival activities and are involved in a variety of biological processes including embryonic development, cell growth, morphogenesis, tissue repair, tumor growth and invasion.[6] FGFs act through a family of four FGF receptors. Binding is complicated and requires both interaction of the FGF molecule with an FGF receptor and binding to heparin through a heparin binding domain. Endocrine FGFs lack a heparin binding domain and thus can be released into the circulation.
FGF21 is a hepatokine – i.e., a hormone secreted by the liver – that regulates simple sugar intake and preferences for sweet foods via signaling through FGF21 receptors in the paraventricular nucleus of the hypothalamus and correlates with reduced dopamine neurotransmission within the nucleus accumbens.[8][9][10]
A single-nucleotide polymorphism of the FGF21 gene – the FGF21 rs838133 variant (frequency 44.7%) – has been identified as a genetic mechanism responsible for the sweet tooth behavioral phenotype, a trait associated with cravings for sweets and high sugar consumption, in both humans and mice.[11][12][13]
Regulation[edit]
FGF21 is specifically induced by mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase 2 (HMGCS2) activity. The oxidized form of ketone bodies (acetoacetate) in a cultured medium also induced FGF21, possibly via a sirtuin 1 (SIRT1)-dependent mechanism.[14] HMGCS2 activity has also been shown to be increased by deacetylation of lysines 310, 447, and 473 via SIRT3 in the mitochondria.[15]
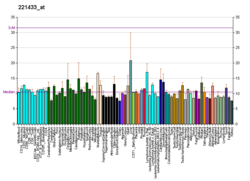
While FGF21 is expressed in numerous tissues, including liver, brown adipose tissue, white adipose tissue (WAT) and pancreas, circulating levels of FGF21 are derived specifically from the liver in mice.[16] In liver FGF21 expression is regulated by PPARα[17] and levels rise substantially with both fasting and consumption of ketogenic diets.
Liver X receptor (LXR) represses FGF21 in humans via an LXR response element located from -37 to -22 bp on the human FGF21 promoter.[18]
Function[edit]
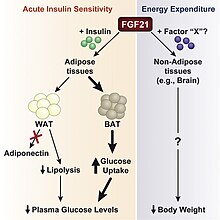
FGF21 stimulates glucose uptake in adipocytes but not in other cell types.[19] This effect is additive to the activity of insulin. FGF21 treatment of adipocytes is associated with phosphorylation of FRS2, a protein linking FGF receptors to the Ras/MAP kinase pathway. FGF21 injection in ob/ob mice results in an increase in Glut1 in adipose tissue. FGF21 also protects animals from diet-induced obesity when overexpressed in transgenic mice and lowers blood glucose and triglyceride levels when administered to diabetic rodents.[19] Treatment of animals with FGF21 results in increased energy expenditure, fat utilization and lipid excretion.[20]
β-Klotho (KLB) functions as a cofactor essential for FGF21 activity.[21]
In cows plasma FGF21 was nearly undetectable in late pregnancy (LP), peaked at parturition, and then stabilized at lower, chronically elevated concentrations during early lactation (EL). Plasma FGF21 was similarly increased in the absence of parturition when an energy-deficit state was induced by feed restricting late-lactating dairy cows, implicating energy insufficiency as a cause of chronically elevated FGF21 in EL. The liver was the major source of plasma FGF21 in early lactation with little or no contribution by WAT, skeletal muscle, and mammary gland. Meaningful expression of the FGF21 coreceptor β-Klotho was restricted to liver and WAT in a survey of 15 tissues that included the mammary gland. Expression of β-Klotho and its subset of interacting FGF receptors was modestly affected by the transition from LP to EL in liver but not in WAT.[22]
Clinical significance[edit]
Serum FGF-21 levels were significantly increased in patients with type 2 diabetes mellitus (T2DM) which may indicate a role in the pathogenesis of T2DM.[23] Elevated levels also correlate with liver fat content in non-alcoholic fatty liver disease[24] and positively correlate with BMI in humans suggesting obesity as a FGF21-resistant state.[25]
A single-nucleotide polymorphism (SNP) of the FGF21 gene – the FGF21 rs838133 variant (frequency 44.7%) – has been identified as a genetic mechanism responsible for the sweet tooth behavioral phenotype, a trait associated with cravings for sweets and high sugar consumption, in both humans and mice.[11][12][13]
Animal studies[edit]
Mice lacking FGF21 fail to fully induce PGC-1α expression in response to a prolonged fast and have impaired gluconeogenesis and ketogenesis.[26]
FGF21 stimulates phosphorylation of fibroblast growth factor receptor substrate 2 and ERK1/2 in the liver. Acute FGF21 treatment induced hepatic expression of key regulators of gluconeogenesis, lipid metabolism, and ketogenesis including glucose-6-phosphatase, phosphoenol pyruvate carboxykinase, 3-hydroxybutyrate dehydrogenase type 1, and carnitine palmitoyltransferase 1α. In addition, injection of FGF21 was associated with decreased circulating insulin and free fatty acid levels. FGF21 treatment induced mRNA and protein expression of PGC-1α, but in mice PGC-1α expression was not necessary for the effect of FGF21 on glucose metabolism.[27]
In mice FGF21 is strongly induced in liver by prolonged fasting via PPAR-alpha and in turn induces the transcriptional coactivator PGC-1α and stimulates hepatic gluconeogenesis, fatty acid oxidation, and ketogenesis. FGF21 also blocks somatic growth and sensitizes mice to a hibernation-like state of torpor, playing a key role in eliciting and coordinating the adaptive starvation response. FGF21 expression is also induced in white adipose tissue by PPAR-gamma, which may indicate it also regulates metabolism in the fed state.[28] FGF21 is induced in both rodents and humans consuming a low protein diet.[29][30] FGF21 expression is also induced by diets with reduced levels of the essential dietary amino acids methionine[31][32] or threonine,[33] or with reduced levels of branched-chain amino acids.[34]
Activation of AMPK and SIRT1 by FGF21 in adipocytes enhanced mitochondrial oxidative capacity as demonstrated by increases in oxygen consumption, citrate synthase activity, and induction of key metabolic genes. The effects of FGF21 on mitochondrial function require serine/threonine kinase 11 (STK11/LKB1), which activates AMPK. Inhibition of AMPK, SIRT1, and PGC-1α activities attenuated the effects of FGF21 on oxygen consumption and gene expression, indicating that FGF21 regulates mitochondrial activity and enhances oxidative capacity through an LKB1-AMPK-SIRT1-PGC-1α-dependent mechanism in adipocytes, resulting in increased phosphorylation of AMPK, increased cellular NAD+ levels and activation of SIRT1 and deacetylation of SIRT1 targets PGC-1α and histone 3.[35]
Acutely, the rise in FGF21 in response to alcohol consumption inhibits further drinking. Chronically, the rise in FGF21 expression in the liver may protect against liver damage.[7]
References[edit]
- ^ a b c GRCh38: Ensembl release 89: ENSG00000105550 - Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000030827 - Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Nishimura T, Nakatake Y, Konishi M, Itoh N (June 2000). "Identification of a novel FGF, FGF-21, preferentially expressed in the liver". Biochimica et Biophysica Acta (BBA) - Gene Structure and Expression. 1492 (1): 203–6. doi:10.1016/S0167-4781(00)00067-1. PMID 10858549.
- ^ a b "Entrez Gene: FGF21 fibroblast growth factor 21".
- ^ a b BonDurant LD, Potthoff MJ (May 2018). "Fibroblast Growth Factor 21: A Versatile Regulator of Metabolic Homeostasis". Annu Rev Nutr. 38: 173–196. doi:10.1146/annurev-nutr-071816-064800. PMC 6964258. PMID 29727594.
- ^ von Holstein-Rathlou S, BonDurant LD, Peltekian L, Naber MC, Yin TC, Claflin KE, Urizar AI, Madsen AN, Ratner C, Holst B, Karstoft K, Vandenbeuch A, Anderson CB, Cassell MD, Thompson AP, Solomon TP, Rahmouni K, Kinnamon SC, Pieper AA, Gillum MP, Potthoff MJ (February 2016). "FGF21 Mediates Endocrine Control of Simple Sugar Intake and Sweet Taste Preference by the Liver". Cell Metabolism. 23 (2): 335–43. doi:10.1016/j.cmet.2015.12.003. PMC 4756759. PMID 26724858.
- ^ Talukdar S, Owen BM, Song P, Hernandez G, Zhang Y, Zhou Y, Scott WT, Paratala B, Turner T, Smith A, Bernardo B, Müller CP, Tang H, Mangelsdorf DJ, Goodwin B, Kliewer SA (February 2016). "FGF21 Regulates Sweet and Alcohol Preference". Cell Metabolism. 23 (2): 344–9. doi:10.1016/j.cmet.2015.12.008. PMC 4749404. PMID 26724861.
- ^ Søberg S, Sandholt CH, Jespersen NZ, Toft U, Madsen AL, von Holstein-Rathlou S, Grevengoed TJ, Christensen KB, Bredie WL, Potthoff MJ, Solomon TP, Scheele C, Linneberg A, Jørgensen T, Pedersen O, Hansen T, Gillum MP, Grarup N (May 2017). "FGF21 Is a Sugar-Induced Hormone Associated with Sweet Intake and Preference in Humans". Cell Metabolism. 25 (5): 1045–1053.e6. doi:10.1016/j.cmet.2017.04.009. PMID 28467924.
- ^ a b Frayling TM, Beaumont RN, Jones SE, Yaghootkar H, Tuke MA, Ruth KS, Casanova F, West B, Locke J, Sharp S, Ji Y, Thompson W, Harrison J, Etheridge AS, Gallins PJ, Jima D, Wright F, Zhou Y, Innocenti F, Lindgren CM, Grarup N, Murray A, Freathy RM, Weedon MN, Tyrrell J, Wood AR (April 2018). "A Common Allele in FGF21 Associated with Sugar Intake Is Associated with Body Shape, Lower Total Body-Fat Percentage, and Higher Blood Pressure". Cell Reports. 23 (2): 327–336. doi:10.1016/j.celrep.2018.03.070. PMC 5912948. PMID 29641994.
- ^ a b Greenhill C (July 2017). "Liver: FGF21 - the cause of having a 'sweet tooth'?". Nature Reviews. Endocrinology. 13 (7): 378. doi:10.1038/nrendo.2017.62. PMID 28497814. S2CID 3906326.
- ^ a b Geach T (March 2016). "Neuroendocrinology: FGF21 influences a 'sweet tooth' in mice". Nature Reviews. Endocrinology. 12 (3): 123. doi:10.1038/nrendo.2016.8. PMID 26822924. S2CID 8239766.
- ^ Vilà-Brau A, De Sousa-Coelho AL, Mayordomo C, Haro D, Marrero PF (June 2011). "Human HMGCS2 regulates mitochondrial fatty acid oxidation and FGF21 expression in HepG2 cell line". The Journal of Biological Chemistry. 286 (23): 20423–30. doi:10.1074/jbc.M111.235044. PMC 3121469. PMID 21502324.
- ^ Shimazu T, Hirschey MD, Hua L, Dittenhafer-Reed KE, Schwer B, Lombard DB, Li Y, Bunkenborg J, Alt FW, Denu JM, Jacobson MP, Verdin E (December 2010). "SIRT3 deacetylates mitochondrial 3-hydroxy-3-methylglutaryl CoA synthase 2 and regulates ketone body production". Cell Metabolism. 12 (6): 654–61. doi:10.1016/j.cmet.2010.11.003. PMC 3310379. PMID 21109197.
- ^ Markan KR, Naber MC, Ameka MK, Anderegg MD, Mangelsdorf DJ, Kliewer SA, Mohammadi M, Potthoff MJ (December 2014). "Circulating FGF21 is liver derived and enhances glucose uptake during refeeding and overfeeding". Diabetes. 63 (12): 4057–63. doi:10.2337/db14-0595. PMC 4238010. PMID 25008183.
- ^ Grabacka M, Pierzchalska M, Dean M, Reiss K (2016). "Regulation of Ketone Body Metabolism and the Role of PPARα". International Journal of Molecular Sciences. 17 (12): E2093. doi:10.3390/ijms17122093. PMC 5187893. PMID 27983603.
- ^ Uebanso T, Taketani Y, Yamamoto H, Amo K, Tanaka S, Arai H, Takei Y, Masuda M, Yamanaka-Okumura H, Takeda E (July 2012). "Liver X receptor negatively regulates fibroblast growth factor 21 in the fatty liver induced by cholesterol-enriched diet". The Journal of Nutritional Biochemistry. 23 (7): 785–90. doi:10.1016/j.jnutbio.2011.03.023. PMID 21889884.
- ^ a b Kharitonenkov A, Shiyanova TL, Koester A, Ford AM, Micanovic R, Galbreath EJ, Sandusky GE, Hammond LJ, Moyers JS, Owens RA, Gromada J, Brozinick JT, Hawkins ED, Wroblewski VJ, Li DS, Mehrbod F, Jaskunas SR, Shanafelt AB (June 2005). "FGF-21 as a novel metabolic regulator". The Journal of Clinical Investigation. 115 (6): 1627–35. doi:10.1172/JCI23606. PMC 1088017. PMID 15902306.
- ^ Coskun T, Bina HA, Schneider MA, Dunbar JD, Hu CC, Chen Y, Moller DE, Kharitonenkov A (December 2008). "Fibroblast growth factor 21 corrects obesity in mice". Endocrinology. 149 (12): 6018–27. doi:10.1210/en.2008-0816. PMID 18687777.
- ^ Ogawa Y, Kurosu H, Yamamoto M, Nandi A, Rosenblatt KP, Goetz R, Eliseenkova AV, Mohammadi M, Kuro-o M (May 2007). "BetaKlotho is required for metabolic activity of fibroblast growth factor 21". Proceedings of the National Academy of Sciences of the United States of America. 104 (18): 7432–7. Bibcode:2007PNAS..104.7432O. doi:10.1073/pnas.0701600104. PMC 1855074. PMID 17452648.
- ^ Schoenberg KM, Giesy SL, Harvatine KJ, Waldron MR, Cheng C, Kharitonenkov A, Boisclair YR (December 2011). "Plasma FGF21 is elevated by the intense lipid mobilization of lactation". Endocrinology. 152 (12): 4652–61. doi:10.1210/en.2011-1425. PMID 21990311.
- ^ Cheng X, Zhu B, Jiang F, Fan H (2011). "Serum FGF-21 levels in type 2 diabetic patients". Endocrine Research. 36 (4): 142–8. doi:10.3109/07435800.2011.558550. PMID 21973233. S2CID 24454698.
- ^ Yan H, Xia M, Chang X, Xu Q, Bian H, Zeng M, Rao S, Yao X, Tu Y, Jia W, Gao X (2011). "Circulating fibroblast growth factor 21 levels are closely associated with hepatic fat content: a cross-sectional study". PLOS ONE. 6 (9): e24895. Bibcode:2011PLoSO...624895Y. doi:10.1371/journal.pone.0024895. PMC 3174975. PMID 21949781.
- ^ Kralisch S, Fasshauer M (July 2011). "Fibroblast growth factor 21: effects on carbohydrate and lipid metabolism in health and disease". Current Opinion in Clinical Nutrition and Metabolic Care. 14 (4): 354–9. doi:10.1097/MCO.0b013e328346a326. PMID 21505329. S2CID 45095074.
- ^ Potthoff MJ, Inagaki T, Satapati S, Ding X, He T, Goetz R, Mohammadi M, Finck BN, Mangelsdorf DJ, Kliewer SA, Burgess SC (June 2009). "FGF21 induces PGC-1alpha and regulates carbohydrate and fatty acid metabolism during the adaptive starvation response". Proceedings of the National Academy of Sciences of the United States of America. 106 (26): 10853–8. Bibcode:2009PNAS..10610853P. doi:10.1073/pnas.0904187106. PMC 2705613. PMID 19541642.
- ^ Fisher FM, Estall JL, Adams AC, Antonellis PJ, Bina HA, Flier JS, Kharitonenkov A, Spiegelman BM, Maratos-Flier E (August 2011). "Integrated regulation of hepatic metabolism by fibroblast growth factor 21 (FGF21) in vivo". Endocrinology. 152 (8): 2996–3004. doi:10.1210/en.2011-0281. PMC 3138239. PMID 21712364.
- ^ Kliewer SA, Mangelsdorf DJ (January 2010). "Fibroblast growth factor 21: from pharmacology to physiology". The American Journal of Clinical Nutrition. 91 (1): 254S–257S. doi:10.3945/ajcn.2009.28449B. PMC 2793111. PMID 19906798.
- ^ Laeger T, Henagan TM, Albarado DC, Redman LM, Bray GA, Noland RC, Münzberg H, Hutson SM, Gettys TW, Schwartz MW, Morrison CD (September 2014). "FGF21 is an endocrine signal of protein restriction". The Journal of Clinical Investigation. 124 (9): 3913–22. doi:10.1172/JCI74915. PMC 4153701. PMID 25133427.
- ^ Fontana L, Cummings NE, Arriola Apelo SI, Neuman JC, Kasza I, Schmidt BA, Cava E, Spelta F, Tosti V, Syed FA, Baar EL, Veronese N, Cottrell SE, Fenske RJ, Bertozzi B, Brar HK, Pietka T, Bullock AD, Figenshau RS, Andriole GL, Merrins MJ, Alexander CM, Kimple ME, Lamming DW (July 2016). "Decreased Consumption of Branched-Chain Amino Acids Improves Metabolic Health". Cell Reports. 16 (2): 520–530. doi:10.1016/j.celrep.2016.05.092. PMC 4947548. PMID 27346343.
- ^ Lees EK, Król E, Grant L, Shearer K, Wyse C, Moncur E, Bykowska AS, Mody N, Gettys TW, Delibegovic M (October 2014). "Methionine restriction restores a younger metabolic phenotype in adult mice with alterations in fibroblast growth factor 21". Aging Cell. 13 (5): 817–27. doi:10.1111/acel.12238. PMC 4331744. PMID 24935677.
- ^ Yu D, Yang SE, Miller BR, Wisinski JA, Sherman DS, Brinkman JA, Tomasiewicz JL, Cummings NE, Kimple ME, Cryns VL, Lamming DW (January 2018). "Short-term methionine deprivation improves metabolic health via sexually dimorphic, mTORC1-independent mechanisms". FASEB Journal. 32 (6): 3471–3482. doi:10.1096/fj.201701211R. PMC 5956241. PMID 29401631.
- ^ Yap, Yann W.; Rusu, Patricia M.; Chan, Andrea Y.; Fam, Barbara C.; Jungmann, Andreas; Solon-Biet, Samantha M.; Barlow, Christopher K.; Creek, Darren J.; Huang, Cheng; Schittenhelm, Ralf B.; Morgan, Bruce (June 9, 2020). "Restriction of essential amino acids dictates the systemic metabolic response to dietary protein dilution". Nature Communications. 11 (1): 2894. Bibcode:2020NatCo..11.2894Y. doi:10.1038/s41467-020-16568-z. ISSN 2041-1723. PMC 7283339. PMID 32518324.
- ^ Cummings NE, Williams EM, Kasza I, Konon EN, Schaid MD, Schmidt BA, Poudel C, Sherman DS, Yu D, Arriola Apelo SI, Cottrell SE, Geiger G, Barnes ME, Wisinski JA, Fenske RJ, Matkowskyj KA, Kimple ME, Alexander CM, Merrins MJ, Lamming DW (February 2018). "Restoration of metabolic health by decreased consumption of branched-chain amino acids". The Journal of Physiology. 596 (4): 623–645. doi:10.1113/JP275075. PMC 5813603. PMID 29266268.
- ^ Chau MD, Gao J, Yang Q, Wu Z, Gromada J (July 2010). "Fibroblast growth factor 21 regulates energy metabolism by activating the AMPK-SIRT1-PGC-1alpha pathway". Proceedings of the National Academy of Sciences of the United States of America. 107 (28): 12553–8. Bibcode:2010PNAS..10712553C. doi:10.1073/pnas.1006962107. PMC 2906565. PMID 20616029.
Further reading[edit]
- Chen WW, Li L, Yang GY, Li K, Qi XY, Zhu W, Tang Y, Liu H, Boden G (January 2008). "Circulating FGF-21 levels in normal subjects and in newly diagnose patients with Type 2 diabetes mellitus". Experimental and Clinical Endocrinology & Diabetes. 116 (1): 65–8. doi:10.1055/s-2007-985148. PMID 17926232. S2CID 260134526.
- Kharitonenkov A, Wroblewski VJ, Koester A, Chen YF, Clutinger CK, Tigno XT, Hansen BC, Shanafelt AB, Etgen GJ (February 2007). "The metabolic state of diabetic monkeys is regulated by fibroblast growth factor-21". Endocrinology. 148 (2): 774–81. doi:10.1210/en.2006-1168. PMID 17068132.
- Zhang Z, Henzel WJ (October 2004). "Signal peptide prediction based on analysis of experimentally verified cleavage sites". Protein Science. 13 (10): 2819–24. doi:10.1110/ps.04682504. PMC 2286551. PMID 15340161.
- Popovici C, Conchonaud F, Birnbaum D, Roubin R (September 2004). "Functional phylogeny relates LET-756 to fibroblast growth factor 9". The Journal of Biological Chemistry. 279 (38): 40146–52. doi:10.1074/jbc.M405795200. PMID 15199049.
- Youm YH, Horvath TL, Mangelsdorf DJ, Kliewer SA, Dixit VD (January 2016). "Prolongevity hormone FGF21 protects against immune senescence by delaying age-related thymic involution". Proceedings of the National Academy of Sciences of the United States of America. 113 (4): 1026–31. Bibcode:2016PNAS..113.1026Y. doi:10.1073/pnas.1514511113. PMC 4743827. PMID 26755598.
External links[edit]
- fibroblast+growth+factor+21 at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- "FGF21". Information Hyperlinked over Proteins. ihop-net.org. Retrieved August 12, 2008.
- "FGF21". Gene Cards. Weizmann Institute of Science. Retrieved August 12, 2008.
- Got a sweet tooth? Blame your liver Phys.org, 2017
This article incorporates text from the United States National Library of Medicine, which is in the public domain.